About SYNAGIS® (palivizumab)
SYNAGIS has both clinical trial results and more than 25 years of real-world evidence in infants at the highest risk for severe RSV disease. SYNAGIS reduces RSV hospitalizations and the severity of those hospitalizations.1*
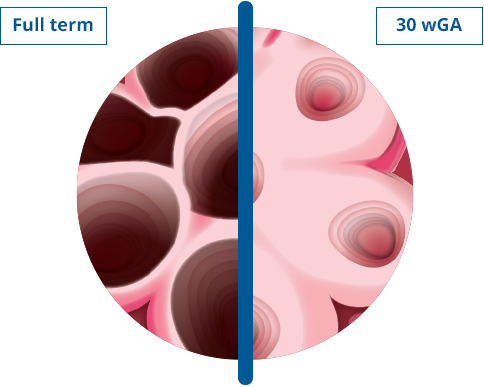
Identify your highest-risk patients, including very preterm infants and children with bronchopulmonary dysplasia (BPD) or hemodynamically significant congenital heart disease (HS-CHD). Provide them with proven protection against severe RSV disease with SYNAGIS.1
*In the pivotal IMpact-RSV study of preterm children with and without BPD, the RSV hospitalization rate was 4.8% in the SYNAGIS group and 10.6% in the placebo group (P<0.001).2

SYNAGIS is a monoclonal antibody that protects the highest-risk infants against severe RSV disease. SYNAGIS has more than 25 years of real-world evidence and proven protection against severe RSV disease in the highest-risk populations, including very preterm infants <29 wGA and children with BPD or HS-CHD.1
SYNAGIS is a monoclonal antibody that helps neutralize RSV activity by binding to the F protein on the surface of RSV to inhibit fusion of the virus to the cell membrane. SYNAGIS also inhibits cell-to-cell fusion, which in turn prevents both viral penetration and syncytia formation—inhibiting RSV replication.1
View the SYNAGIS MOA video
SYNAGIS has more than 25 years of real-world evidence, with proven protection against severe RSV disease in the highest-risk populations, including very preterm infants <29 wGA and children with BPD or HS-CHD.1
In the pivotal IMpact-RSV trial of preterm infants with and without BPD, SYNAGIS reduced the rate of RSV hospitalizations by 55% vs placebo.1,2
SYNAGIS also reduced the severity of those hospitalizations. Compared with patients receiving placebo, those receiving SYNAGIS had 42% fewer days of RSV hospitalization (per 100 children: 62.6 days with placebo vs 36.4 days with SYNAGIS; P<0.001), a 57% lower rate of ICU admissions (3.0% with placebo vs 1.3% with SYNAGIS; P=0.026), and 40% fewer days with increased supplemental oxygen (per 100 children: 50.6 days with placebo vs 30.3 days with SYNAGIS; P<0.001). The placebo and SYNAGIS groups did not show significant differences in incidence of mechanical ventilation (0.2% vs 0.7%, P=0.280) or total days of mechanical ventilation (1.7 days vs 8.4 days, P=0.210). ICU total days were 12.7 with placebo and 13.3 with SYNAGIS (P=0.023).2
In the pivotal Feltes trial of children with HS-CHD, SYNAGIS reduced the rate of RSV hospitalizations by 45% vs placebo.1,3
SYNAGIS also reduced the severity of those hospitalizations. Compared with patients receiving placebo, those receiving SYNAGIS had 56% fewer days of RSV hospitalization (per 100 children: 129 days for placebo vs 57.4 days with SYNAGIS; P=0.003) and 73% fewer days with increased supplemental oxygen (per 100 children: 101.5 days for placebo vs 27.9 days with SYNAGIS; P=0.014). The placebo and SYNAGIS groups did not show statistically significant differences in incidence of RSV-related ICU admissions (3.7% vs 2.0%, P=0.094), total days of RSV-related ICU stays per 100 children (71.2 days vs 15.9 days, P=0.80), incidence of RSV-related mechanical ventilation (2.2% vs 1.3%, P=0.282), or total days of RSV-related mechanical ventilation per 100 children (54.7 days vs 6.5 days, P=0.224).3
SYNAGIS also reduced RSVH severity among very preterm infants in a real-world study. A retrospective observational cohort study conducted over 17 RSV seasons among medically fragile, very preterm infants <29 wGA found that outpatient administration of SYNAGIS reduced RSVH-related length of stay, rates of ICU admission, ICU length of stay, and rates of mechanical ventilation.4
In this real-world study, commercially insured infants who received SYNAGIS (N=183) compared with those who did not receive SYNAGIS (N=96) had a significantly reduced mean length of hospital stay (7.4 days vs 9.0 days; P<0.001) and significantly reduced mean length of ICU stay (9.5 days vs 13.7 days; P=0.008). There was no significant difference between groups in percentage admitted to the ICU (33.9% with SYNAGIS vs 36.5% without SYNAGIS; P=0.667) or in percentage who required mechanical ventilation (1.6% with SYNAGIS vs 4.2% without SYNAGIS; P=0.200).4
In the same study, Medicaid-insured infants who received SYNAGIS (N=707) vs those who did not receive SYNAGIS (N=447) had a significantly reduced mean length of hospital stay (8.1 days vs 10.8 days; P=0.019), a significantly lower percentage admitted to the ICU (35.6% vs 44.7%; P=0.002), and a significantly lower percentage requiring mechanical ventilation (6.0% vs 2.8%; P=0.007). There was no significant difference between groups in mean length of ICU stay (12.8 days vs 14.7 days; P=0.191).4
Learn more about SYNAGIS efficacy
With SYNAGIS, you dose every 28 to 30 days, giving you the ability to protect your highest-risk infants optimally throughout the season, reducing RSV hospitalizations and RSVH severity.1-4 The SYNAGIS dosing regimen allows you to dose-adjust by weight as an infant or child grows—each dose is determined by weight at the time of administration for that infant. In addition, you can adjust dosing when the RSV season is longer than usual or interseasonal RSV activity occurs.1
Learn more about SYNAGIS dosing
In the pivotal trials combined, AEs occurring at a rate of >10% and ≥1% more frequently with SYNAGIS than with placebo were fever and rash.1 In the pivotal IMpact-RSV trial of preterm infants with and without BPD, similar percentages of children experienced AEs in the placebo and SYNAGIS groups.2 In the pivotal Feltes trial of children with HS-CHD, few AEs were reported at an absolute incidence ≥1% higher in the SYNAGIS group than in the placebo group.3
View the safety data for SYNAGIS
CONTRAINDICATIONS
SYNAGIS is contraindicated in children who have had a previous significant hypersensitivity reaction to SYNAGIS.1
WARNINGS AND PRECAUTIONS
Cases of anaphylaxis and anaphylactic shock, including fatal cases, have been reported following initial exposure or re-exposure to SYNAGIS. Other acute hypersensitivity reactions, which may be severe, have also been reported on initial exposure or re-exposure to SYNAGIS. If a significant hypersensitivity reaction occurs with SYNAGIS, its use should be permanently discontinued. If anaphylaxis or other significant hypersensitivity reaction occurs, administer appropriate medications (eg, epinephrine) and provide supportive care as required. If a mild hypersensitivity reaction occurs, clinical judgment should be used regarding cautious readministration of SYNAGIS.1
For children with BPD that required medical treatment within the previous 6 months and who are ≤24 months of age at the beginning of the RSV season or for children with HS-CHD who are ≤24 months of age at the beginning of the RSV season, SYNAGIS offers protection during the second RSV season.1
There are no data to support the use of SYNAGIS in conjunction with other RSV prevention modalities within the same RSV season.
SYNAGIS can be ordered through a Specialty Pharmacy or Specialty Distributors.
Mechanism of Action (MOA)
- SYNAGIS is a monoclonal antibody that provides seasonal immunoprophylaxis1
- SYNAGIS is not a vaccine
View the video
ICU=intensive care unit; RSV=respiratory syncytial virus; RSVH=respiratory syncytial virus hospitalization; wGA=weeks gestational age.
REFERENCES: 1. SYNAGIS (palivizumab) [prescribing information]. Waltham, MA: Sobi, Inc. 2021. 2. The IMpact-RSV Study Group. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics. 1998;102(3):531-537. 3. Feltes TF, Cabalka AK, Meissner HC, et al. Palivizumab prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant congenital heart disease. J Pediatr. 2003;143(4):532-540. 4. Packnett ER, Winer IH, Larkin H, et al. RSV-related hospitalization and outpatient palivizumab use in very preterm (born at <29 wGA) infants: 2003-2020. Hum Vaccin Immunother. 2022;18(6):2140533. doi:10.1080/21645515.2022.2140533
All imagery is for illustrative purposes only.